Nutrition Education

At the University of South Florida Morsani College of Medicine, nutrition is recognized as a foundational pillar of health, disease prevention, and clinical care. Throughout the curriculum and within Scholarly Concentrations, interest groups, student organizations and interprofessional activities, students are trained to understand the role of nutrition across the lifespan and its impact on chronic disease prevention, metabolic health, and immune function. Here are some of the ways students learn about nutrition and are prepared to deliver comprehensive, patient-centered care.
Time for the nation's doctors to treat food as medicine
Read Dr. Lockwood's blog as well as opinion column that was published in the Feb. 25 edition of the Tampa Bay Times.
Call to Action
Mission
To prepare future physicians to integrate evidence-based nutrition into patient care across the continuum of health and disease through a longitudinal, clinically integrated curriculum that develops the knowledge, skills, and professional judgment essential for prevention, treatment, and chronic disease management.
Vision
To graduate physicians who integrate nutrition seamlessly into clinical reasoning, patient counseling, and professional identity. Through deliberate, longitudinal integration across basic science and clinical training, our curriculum emphasizes practical application, accountability, and relevance—advancing excellence in patient-centered care while preparing physicians for real-world practice.

Institutional Commitment
The USF Morsani College of Medicine is committed to supporting the continued expansion of nutrition and lifestyle medicine education through targeted, sustainable investments. The College will provide dedicated faculty leadership to coordinate and integrate nutrition and lifestyle medicine content across the curriculum, working with course directors to ensure coherent, non-redundant coverage aligned with institutional priorities.
Support will also include continued development of experiential culinary medicine education and access to high-quality, evidence-based instructional resources to promote consistency, efficiency, and educational quality. Together, these focused investments will ensure that nutrition education is integrated, accountable, and sustainable within the existing MD curriculum and ensures that MCOM is a leader in nutrition education nationally..




Nutrition Curriculum
-
Nutrition education at USF MCOM is currently delivered across all four years of the MD curriculum through a combination of required coursework, clinical experiences, and emerging enrichment opportunities. Nutrition education at USF MCOM is integrated longitudinally across all four years of the MD curriculum rather than delivered as a stand-alone course. This approach ensures that students encounter nutrition concepts in basic science, clinical skills training, and real patient care settings, reinforcing application across the continuum of medical education.
During the 2025–26 academic year, students receive 36 hours of nutrition instruction distributed longitudinally across the curriculum. In addition, the College has a well-established Nutrition Scholarly Concentration to support deeper student engagement in nutrition-related scholarship. A pilot culinary medicine experience, led by a chef educator, is also underway to explore experiential approaches to nutrition education.
At present, the majority of nutrition competencies identified in the Eisenberg consensus statement are addressed within the curriculum in some form. These include core, patient-facing areas such as nutrition assessment using history, physical examination, and laboratory data; recognition of malnutrition and nutrition-related clinical signs; obesity and metabolic disease counseling; food allergy and intolerance; drug–nutrient interactions; micronutrient deficiencies; use of evidence-based dietary guidance; integration of nutrition into patient care; and interpretation of continuous glucose monitoring data in diabetic and metabolic patients. These topics represent the highest-value components of nutrition education, directly influencing diagnosis, treatment, and outcomes in common chronic diseases.
-
Nutrition content is incorporated throughout required coursework and clinical experiences to ensure that students achieve program objectives related to patient care, prevention, and chronic disease management. Instruction is mapped to course and session-level learning objectives and assessed within existing curricular structures.
This integrated model supports accreditation expectations by demonstrating where and how nutrition is taught across the curriculum, providing sufficient instructional time distributed across multiple phases of training, and ensuring nutrition education is linked to clinical reasoning, patient counseling, and real-world application.
-
Nutrition learning objectives were developed through a structured review of nationally recognized consensus work and federal guidance. Initial objectives were informed by the 2024 JAMA Network Open consensus statement led by Eisenberg et al., which used a modified Delphi process to identify core nutrition competencies for undergraduate and graduate medical education, emphasizing foundational knowledge, assessment, communication skills, interprofessional collaboration, and appropriate referral.
These objectives were then advanced and refined to align with the U.S. Department of Health and Human Services Medical Education Nutrition Competency Framework, which expands upon the consensus work by organizing 71 competencies across ten domains and providing competency-based hour equivalents to support curriculum planning and longitudinal integration.
Together, these frameworks guided the development of objectives that are evidence-informed, developmentally sequenced, and integrated across the curriculum while allowing flexibility for institutional prioritization and ongoing refinement. These competencies and objectives have been approved by the USF MCOM curriculum committee.
-
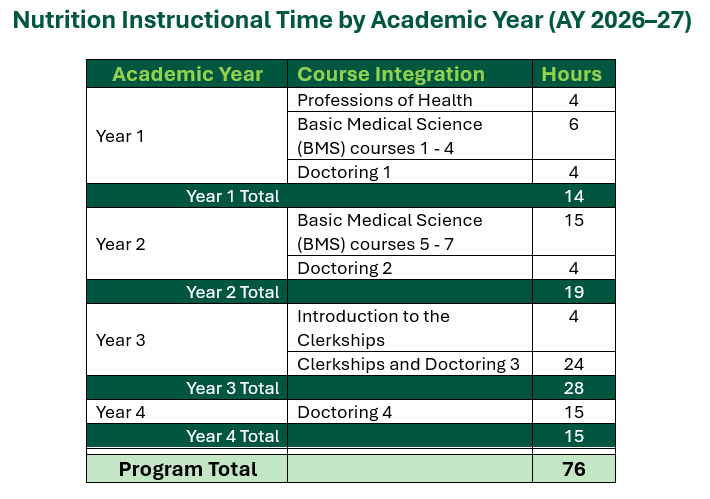
During the 2026–27 academic year, students will receive a total of 76 hours of required nutrition instruction embedded within existing courses and clerkships
-
- Nutritional content of foods, macronutrients and micronutrients
- Pathological states affecting nutrient absorption
- Identifies nutrient deficiencies, recommends foods/supplements
- Difference between food allergies and intolerance including gluten
- Energy and nutrient requirements across lifespan
- Drug-nutrient interactions
- Nutritional differences: minimally processed vs highly processed foods
- Interprets nutrition labels and menu labeling
- Clinically assisted nutrition
- Functions of essential nutrients
- Principles of healthy balanced diet per national guidelines
- Evidence-based guidance on healthy beverage consumption
- Mitochondrial metabolism and energy regulation: understand nutrient-driven ATP synthesis and how overnutrition leads to insulin resistance
- Structural components from food: recognize how dietary amino acids, essential fatty acids, and cholesterol build proteins, membranes, and hormones
- Micronutrient cofactors in enzymatic function: master how vitamins and minerals drive reactions and how deficiencies undermine function
- Hormonal regulation through food composition: understand how meal composition affectsGLP-1, CCK, PYY, leptin, and insulin signaling
- Epigenetic modulation through nutrition: comprehend how methyl donors, phytochemicals, and feeding rhythms influence gene expression
- Microbiome-immune crosstalk: understand fiber fermentation producing butyrate for gut integrity and how ultra-processed diets cause dysbiosis
- Cognitive and behavioral nutrition: apply mindful eating practices that enhance hormonal signaling and reduce reward-driven eating
- Food bioavailability and synergies: knowledge of preparation methods enhancing absorption
- Chronobiology and circadian nutrition: understand how meal timing affects nutrient absorption, hormonal rhythms, and metabolic efficiency
- Assesses nutritional status by integrating dietary history, clinical measurements (height, weight, BMI, skeletal muscle mass, visceral fat), and laboratory findings
- Comprehensive nutrition-focused physical examination
- Interprets exam data and biomarkers for malnutrition risk
- Personalized metabolic biomarker interpretation: using fasting insulin levels, oral glucose tolerance testing (OGGT), HOMA-IR, TG:HDL ratio, advanced lipid panels, omega-3 index, and vitamin D to guide interventions
- Continuous glucose monitoring (CGM) interpretation: analyze CGM data patterns to identify glycemic variability and guide dietary modifications and different use cases for specific populations, including diabetic patients
- Early warning sign recognition: interpret nutrition-related symptoms (fatigue, bloating, anxiety) and signs (brittle nails, hair thinning)
- Integrates evidence-based nutrition information into patient care
- Uses behavior change models to counsel patients
- Guides patients on lifelong dietary patterns for chronic disease
- Brief counseling for visceral adiposity/metabolic syndrome
- Motivational interviewing for nutrition change: apply structured interviewing techniques to enhance autonomy and sustainable behavior change
- Food journaling guidance: teach patients to maintain detailed food journals for pattern identification and accountability
- Mindfulness-based eating interventions: implement eating awareness training to improve hormonal signaling
- Patient empowerment and dietary autonomy: foster long-term self-efficacy through education, biomarker monitoring, and collaborative goal-setting
- Interoceptive awareness training: help patients develop awareness of internal hunger/satiety cues to regulate intake naturally
- Works with other health professionals for multidisciplinary nutrition care
- Makes appropriate referrals to support patient health goals
- Health coach and functional nutritionist collaboration: effectively co-manage patients with non-physician experts
- Digital health technology integration: understand and recommend evidence-based wearables and platforms supporting nutrition outcomes
- Screens for food/nutrition needs and patients’ ability to obtain sufficient nutrition, makes appropriate referrals
- Dietary Guidelines analysis: critically evaluate and translate dietary guidelines into clinical practice
- Creates culinary nutrition SMART goals for personal use and patient care
- Meal preparation: prepare minimally processed, whole-food meals emphasizing nutrient density
- Teaching kitchen learning laboratory: participate in multidisciplinary nutrition learning through hands-on cooking
- GLP-1 agonists counseling with diet and lifestyle guidance
- Responsible use of AI for nutrition advice
- Medication-nutrition synergy: guide patients combining medications, surgery, CGM, wearables with lifestyle practices
- Identifies factors affecting personal health and nutrition status
- Modeling patient-centered behaviors: recognize physician self-care behaviors strongly predict patient counseling patterns
- Personal metabolic optimization: apply systems biology principles to own health data to experience clinical protocols68. Toxicology in the food supply: understand the impacts of potential toxicants in the food supply chain
-
-
Nut 1. Integrate evidence-based nutrition science, national dietary guidelines, and clinical evidence to formulate individualized, culturally responsive nutrition recommendations Mapped competencies: 11, 12, 30, 32, 37, 49
-
Nut 2. Perform a comprehensive nutrition assessment including history, exam, and labs Mapped competencies: 22, 23, 24, 27
-
Nut 3. Explain roles, sources, absorption, and metabolism of macro and micronutrients across the lifespan Mapped competencies: 1, 2, 5, 10, 15
-
Nut 4. Analyze effects of disease, medications, and drug–nutrient interactions on nutrition management Mapped competencies: 2, 6, 25, 59
-
Nut 5. Apply behavior change science and SMART goals to guide sustainable dietary change Mapped competencies: 31, 34, 35, 50
-
Nut 6. Provide culturally responsive, empathetic nutrition counseling Mapped competencies: 34, 36, 37, 38
-
Nut 7. Address obesity, eating disorders, emotional eating, and metabolic risk Mapped competencies: 19, 33, 36, 55
-
Nut 8. Screen for and respond to food and nutrition insecurity Mapped competencies: 44
-
Nut 9. Collaborate with dietitians and interprofessional nutrition teams Mapped competencies: 39, 40, 41
-
Nut 10. Use nutrition labels, menus, and food processing classifications to counsel patients Mapped competencies: 7, 8
-
Nut 11. Diagnose and manage food allergies and intolerances Mapped competencies: 4
-
Nut 12. Provide evidence-based pediatric nutrition recommendations Mapped competencies: 5, 11
-
Nut 13. Manage oral, enteral, and parenteral nutrition Mapped competencies: 9
-
Nut 14. Model and reflect on personal nutrition and health behaviors Mapped competencies: 62, 63, 64
-
Nut 15. Use AI and digital tools for nutrition learning and counseling Mapped competencies: 26, 42, 56
-
Nutrition Research & Health Scholarly Concentration
Scholarly Concentrations are structured longitudinal electives where MD students pursue scholarly work in an area of interest. While nutrition is a topic across many of the SC programs, such as biomedical research, community health & wellness, and international medicine, the Nutrition Research & Health scholarly concentration focuses on:
- principles underlying the nutritional sciences,
- the roles of nutrition in the development and progression of specific diseases,
- application of nutritional counseling to promote optimal health and to prevent disease,
- examination of community factors affecting nutrition health,
- intersection of behavioral health and nutrition, and
- contributions of nutrition to the management of specific pathophysiological conditions.
Interprofessional Activities
The 7th Annual Interprofessional Education Day held November 2024 was titled Nutrition: Fueling Health—Why What We Eat Matters to Ourselves, Our Community, Our Patients, and Our Planet. Experts shared insights on nutrition and food insecurity, and teams of students participated in a culinary competition.
At this event it was shared that a future goal is to Integrate culinary medicine into the curriculum to equip students with the knowledge and skills to support healthy eating and enhance the well-being of families, patients, and communities.
Nutrition Education Team
-
Deborah DeWaay, MD, FACP
Deborah DeWaay, MD, FACPSenior Associate Dean, Undergraduate Medical Education -
Clyde Tanner, MSM, ACF-CEC, ACF-CCE
Clyde Tanner, MSM, ACF-CEC, ACF-CCEExecutive Chef -
Karyn Gerstle, MD, MPH, IBCLC
Karyn Gerstle, MD, MPH, IBCLCNutrition Integration Director



