Residency Program
Clinical Curriculum
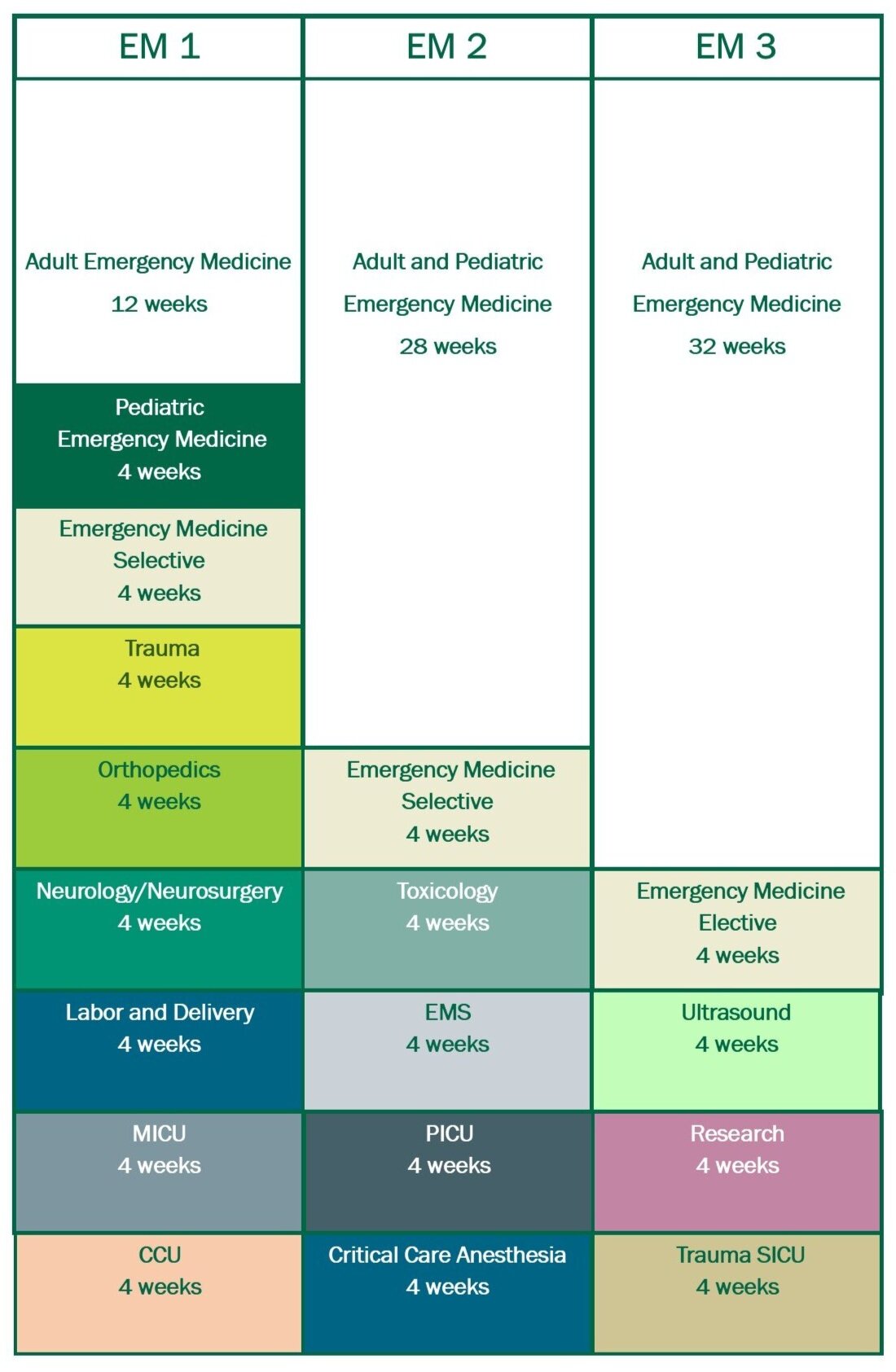
USF EM Clinical Curriculum
PGY-1 Year
- Adult EM (3 months)
- Pediatric EM
- Trauma (ED based)
- Orthopedics (ED based)
- Anesthesia / Ophtho
- Neurology or Neurosurgery
- CCU
- MICU
- OB-GYN
- Selective
Selective Options
- Internal Medicine
- Adult EM
- MICU Select (pulm critical care consult service)
- Teaching selective
- Ultrasound/Procedural
PGY-2 Year
- Emergency Medicine (7 months, includes longitudinal pediatric experience)
- Toxicology
- EMS
- PICU
- MICU select (pulm critical care consult service)
- Selective
Selective Options
- CCU
- MICU select (pulm critical care consult service)
- Adult EM
- EM Critical Care
- Teaching selective
- Ultrasound/procedural
- Gulf to Bay Critical Care
PGY-3 Year
- EM (8 months, includes longitudinal pediatric experience and 1 month at BHP)
- Research/Admin
- Ultrasound
- Trauma-SICU
- Elective
Elective Options
- MICU select (pulm critical care consult service)
- Pediatric EM
- Brandon Healthplex (BHP)
- Other TGH service (Urology, ECMO/LVAD, etc)
- EM Critical Care
- Teaching selective
- Potential for Global Health opportunities
- Independent study
- Ultrasound
- Gulf to Bay Critical Care
Didactic Curriculum
Conference
Our conferences are held on Wednesdays. We meet together for four hours weekly and residents complete an additional hour of asynchronous learning. We work hard every year to adjust conference based on resident feedback and we incorporate multiple educational modalities suitable for adult learners. Our curriculum is designed around core content and a theme for the day. Rather than death by powerpoint, we tend to do shorter lectures, small group discussions, and simulation training. We utilize a combination of virtual and in person education. We enjoy regularly incorporate resources such as EMRAP, EMCRIT, and other current favorites in the EM world.


Toxicology Training
The center is certified as a Regional Poison Center by the American Association of Poison Control Centers and provides coverage to over 7 million residents of central and southwest Florida. The center is located at Tampa General Hospital and our core faculty member, Dr. Justin Arnold, DO, MPH FACEP, FACMT is the Medical Director. In addition, Dr. Diana Dean is the Assistant Director of the and is also a core faculty member. Dr. Alfred Aleguas PharmD, D.ABAT, FAACT is the managing director. The center is staffed 24 hours a day by specially trained nurses, physicians, and pharmacists that receive thousands of inbound calls providing management advice within minutes. Accessible by the national toll-free Poison Help number, 1-800-222-1222, 24/7/365, this regional center is one of 54 certified poison centers covering all of the United States and U.S. possessions.
Residents rotate with Dr. Arnold and the staff of the Florida Poison information center during their toxicology month during the PGY-2 Year. The rotation is also offered to interested 4th year medical students through USF and VSAS.
The toxicology rotation includes:
- Daily poison center case reviews
- In person lectures and didactics
- Asynchronous learning
- Review of important toxicology journal articles
- Participation in a monthly Florida Poison Information Network journal club
- Participation in national case conferences, journal club, and webinars
- Trips to the local zoo and more!
- Opportunities to participate in research and other scholarly activities.
Please visit our Poison Center Tampa and Florida Poison Control websites.
Contact
Justin Arnold, DO, MPH, FACEP, FACMTMedical Director, Florida Poison Information CenterAssistant Professor, University of South Floridajkarnold@usf.edu

Toxicologists Dr. Diana Dean and Dr. Justin Arnold

Pediatrics Training
Our pediatric ED cares for roughly 19,000 patients annually and serves as a level one trauma center and burn facility. The pediatric emergency room is staffed only with pediatric emergency fellowship trained doctors so residents can be certain they are learning from experts in the field. The pediatric ED is located within TGH so residents don't need to worry about traveling to a separate hospital for their pediatric experience. Residents experience community pediatrics at our Brandon Healthplex site. Residents will also rotate through the PICU at Tampa General. TGH serves as a pediatric renal transplant center and is a surgical site for Shriners orthopaedics and spine.
Contact
Jasmine Patterson, MDDirector of the Pediatric Emergency Department

Ultrasound Training
Each resident will be trained in the six primary emergency ultrasound applications (ECHO, gallbladder, kidneys, aorta, 1st trimester pregnancy, FAST) and other secondary applications (DVT, procedural guidance, ocular, musculoskeletal, regional anesthesia, TEE and foreign body removal). Residents in our program complete a minimum of 300 emergency ultrasound examinations. The ultrasound faculty review the residents’ ultrasound images and provide feedback. Images are stored digitally using a state-of-the-art imaging cloud-based system (Q-pathE). Ultrasound rotations are available in the PGY-1 (selective), PGY-2 (selective) and PGY-3 years (required). Our PGY-1 residents participate in a 2-day hands-on ultrasound course held each July. This course covers primary and advanced ultrasound skills and includes a half-day cadaver lab workshop for practicing ultrasound-guided regional anesthesia techniques.
Residents also have the option to participate in an advanced emergency ultrasound track that will prepare them for future roles such as Ultrasound Fellow, Emergency Ultrasound Director, Academic Faculty member, or Ultrasound Course Faculty. The advanced emergency ultrasound curriculum requires participation in and development of departmental ultrasound research, a Grand Rounds case presentation, serving as a QA administrator for junior residents, and the delivery of ultrasound education to junior residents and medical students.
Contact
Allyson Hanson, DO
Residency Ultrasound Director
allyson_hanson@teamhealth.com

Simulation Training
USF Emergency Medicine is proud to provide a world class experiential learning program using high fidelity simulators, standardized patients, task trainers, and cadaver labs. We are excited to offer this broad simulation-based training experience at USF Health's Center for Advanced Medical Learning and Simulation (USF Health CAMLS). At over 90,000 square feet and 3 stories tall, USF Health CAMLS is one of the largest freestanding simulation centers in the United States and is a leader in educational innovation and experiential learning.
Our simulation experience begins during intern orientation, where we focus on the core skills needed to get started in the ED. Our interns enjoy an ultrasound-guided regional anesthesia cadaver lab led by our ultrasound faculty. Throughout the year, our residents engage in monthly simulation-based training sessions that cover high acuity low occurrence cases, procedural skills, communication, and team leadership. The cornerstone of our simulation experience is interprofessional training, and we regularly include the nurses and medics from the emergency department at Tampa General Hospital that we work alongside every day. We even bring in our colleagues from Tampa Fire Rescue from time to time to improve our hand offs and processes surrounding cardiac arrest. We conclude our academic year with an annual advanced procedural skills cadaver lab that covers everything from lateral canthotomies to thoractomies. In addition, every year we host the USF Difficulty AirwayTM Residency Edition course. For those interested in simulation, we offer an elective in simulation for residents. For more information about our simulation program, visit the links below:
- Close Up With Cathy Unruh: April 2018: CAMLS
- USF Health CAMLS Without Walls
- Interprofessional Simulation Based Training USF CAMLS
- CAMLS Fellowship
Contact
Nicole Rettig, MD
Residency Simulation Director
nabdo@usf.edu

EMS Training
The EMS rotation gives residents an opportunity to see prehospital medicine and its impact on our patients. Residents gain insight into the challenges and opportunities that arise when providing medical care outside the brick and mortar of the emergency department, and the way that it affects our patients’ clinical course. Residents go on Advanced Life Support (ALS) ambulance rides with Tampa Fire Rescue, a metropolitan fire-rescue service that began over 125 years ago and receives over 75,000 calls annually. In addition to ambulance ride-alongs, there will be opportunities to ride with a supervisor vehicle and respond to various calls throughout the city.
The rotation also offers the opportunity to ride with Aeromed, Tampa General Hospital’s helicopter EMS service that has bases in Hillsborough, Highlands, Polk, and Charlotte Counties. Aeromed responds to a mix of both scene calls and interfacility transports and practices very high acuity critical care.
The EMS block also includes the chance to participate in event medicine. Tampa Bay is home to some amazing events including road races, parades, festivals, concerts, conventions, and major sporting events including NCAA basketball, NCAA football, NHL and NFL games including the Super Bowl. Our indoor events at the Tampa Bay Convention Center, the Amalie Arena, and Raymond James Stadium can hold tens of thousands and requires ample medical coverage. Residents can serve along with Tampa Fire Rescue for events such as these and learn how events have unique emergency medical needs. For major events, even residents on other rotations could be involved in providing care if there is sufficient need.
Finally, the EMS rotation will provide time for residents to learn the science of prehospital medicine from several faculty that are fellowship-trained in EMS or Disaster Medicine. We will discuss landmark articles that helped improve the delivery of prehospital care and impact the decisions we make when crafting protocols or advising medics. For those interested in pursuing an EMS fellowship, this rotation is only a small part of the mentorship offered before you apply for the match – we will work with you on research and other experiences to make you well-prepared.
Contact
Rachel Semmons, MDEMS Fellowship DirectorAssistant Medical DirectorRachel.semmons@gmail.com