Center of Excellence for Aging & Brain Repair
Repair of The Damaged Blood-CNS-Barriers
Based on Dr. Garbuzova-Davis’ original findings showing alterations to the blood-CNS-barrier in an ALS model of disease and in ALS patients, her team’s current focus is developing cellular and cell-free approaches for barrier repair. The group has been exploring the effects of transplanted human bone marrow endothelial progenitor cells on an animal model of disease. Additionally, extracellular vesicles derived from the same progenitor cells have been investigated as potential cell-free therapeutics for repair of the damaged CNS barrier in ALS. This translational research on barrier repair aims toward eventual restoration of neurovascular unit functionality in patients with ALS or other neurovascular diseases.
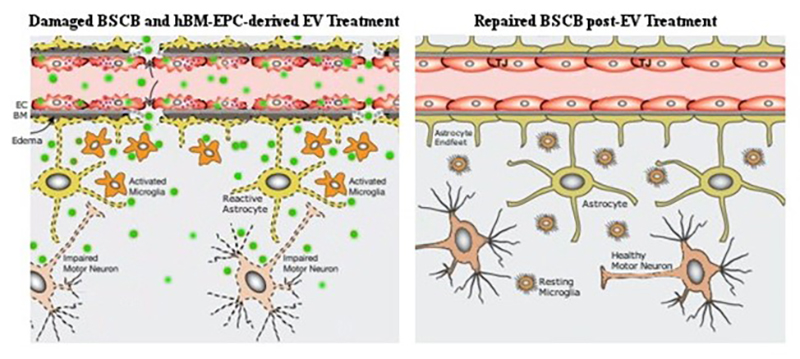
Schematic representation of hBM-EPC-derived extracellular vesicle (EV) effects for blood-spinal cord barrier (BSCB) repair in ALS. (Left image) BSCB damage is characterized by degeneration of ECs and astrocyte end-feet, loss of “tightness” in tight junctions. This damage leads to increased vessel permeability and eventual motor neuron death. Intravenous delivery of the EVs (green) leads to widespread distribution of these vesicles and release of their cargo proteins inside ECs and in spinal cord parenchyma. (Right image) EV treatment restored BSCB integrity by re-establishing EC functionality and other barrier constituents, leading to increased motor neuron survival. EC – endothelial cell, TJ – tight junction, BM – basement membrane.